Agents Can Help Show Diversity of Options
Agents can help show diversity of options, opening up a world of possibilities for users. From travel planning to product recommendations, agents act as personalized guides, curating a selection of options tailored to individual needs and preferences. This exploration delves into how agents can effectively showcase diverse choices, ensuring a richer and more satisfying user experience.
This discussion will cover the fundamental concepts of diversity in options, exploring various methods for presentation, and examining the user-centric approach agents employ to curate the best possible selection. We will also analyze the technical capabilities needed to handle diverse data effectively, along with real-world examples and the impact on user experience.
Defining Diversity of Options
Agent diversity isn’t just about having different-looking agents; it’s about offering a wide array of capabilities and functionalities tailored to various user needs and contexts. A truly diverse agent system recognizes the multifaceted nature of tasks and provides options that cater to specific situations, rather than a one-size-fits-all approach. This allows users to choose the best tool for the job, leading to increased efficiency and satisfaction.A diverse set of options for agents empowers users to choose the most effective approach for a particular task.
This adaptability is crucial in dynamic environments where conditions and requirements change frequently. This adaptability isn’t just about offering different ways to achieve the same outcome; it’s about understanding the nuances of various situations and providing options that cater to specific circumstances.
Agent Types and Diverse Options
Different types of agents are designed to handle diverse tasks and offer varying levels of complexity. The key is recognizing that a diverse set of options is crucial for any agent to be truly effective. Agents aren’t monolithic; their functionality and capabilities should mirror the complexity of the problems they’re intended to solve.
Travel agents are invaluable for showcasing the incredible diversity of travel options, from budget-friendly escapes to luxurious getaways. For example, the recent news of after 8 years Veitch departs NCL highlights how important these professionals are in navigating the complexities of the industry. Ultimately, they’re your best bet for finding the perfect trip, no matter what your needs or desires.
Examples of Diverse Options
Agents can showcase diversity in their options by providing multiple approaches to a problem. For instance, a customer service agent might offer various ways to resolve a complaint: a phone call, email, chat, or a social media message. This flexibility allows the customer to choose the method most convenient for them. Another example includes a travel agent presenting a range of flight options based on price, duration, and layover time, enabling the user to select the best fit for their needs.
Likewise, a research agent could provide multiple sources, varying in depth and specificity, to address a particular research question.
Different Agent Types and Their Capabilities
This section highlights how various types of agents can demonstrate diversity in their offerings. Each agent type will offer unique strengths and capabilities, which are important considerations when determining the most appropriate agent for a given task. For example, a rule-based agent excels at tasks that involve predefined actions, while a learning agent continuously adapts its responses based on user interaction and feedback.
Comparison of Agent Types
| Agent Type | Ability to Present Diverse Options | Strengths | Limitations |
|---|---|---|---|
| Rule-Based Agent | Limited, based on predefined rules | Fast, efficient for specific tasks | Cannot adapt to new or unexpected situations |
| Learning Agent | High, adapts based on user interaction | Flexible, improves with experience | Requires data and time to learn effectively |
| Hybrid Agent | Medium to High, combines rule-based and learning approaches | Balances speed and adaptability | Can be complex to design and implement |
| AI-powered Agent | High, utilizes advanced algorithms and machine learning | Excellent problem-solving and decision-making | Can be expensive and requires significant computational resources |
Methods of Presenting Diverse Options: Agents Can Help Show Diversity Of Options
Presenting a wide array of options effectively is crucial for user satisfaction and informed decision-making. Agents need to go beyond simply listing choices; they must craft a presentation that highlights the unique benefits and potential outcomes of each option. This involves careful consideration of the presentation methods and strategies employed. A well-structured approach can greatly enhance the user experience and empower them to select the most suitable option for their needs.Understanding user preferences and motivations is key to choosing the most effective presentation style.
A presentation method that is intuitive and clear for one user might be confusing or overwhelming for another. Consequently, adaptable and versatile methods are essential. Agents should tailor their approach to the specific situation and the individual user.
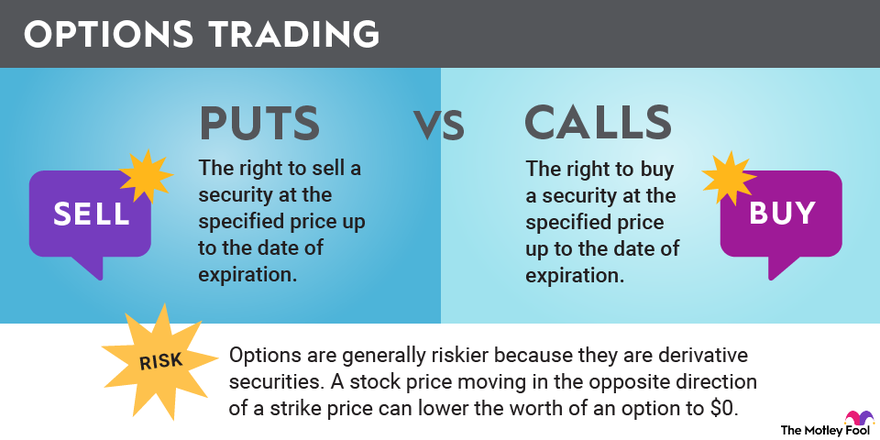
Presentation Strategies for Highlighting Unique Qualities
Different presentation strategies can be used to emphasize the distinct characteristics of each option. A key strategy is to use visuals and compelling descriptions that highlight the unique value proposition of each choice. Examples of strategies include emphasizing key features, using comparative tables, or offering case studies demonstrating the practical applications of each option. Visual aids such as charts, graphs, and images can significantly enhance understanding and engagement.
Comparative Analysis of Presentation Formats
Different presentation formats—lists, grids, summaries, and others—can be employed to effectively showcase the diversity of options. The choice of format should be tailored to the specific needs and characteristics of the options being presented. A simple list might suffice for a small number of straightforward choices, but a more complex format like a grid or summary might be necessary for a large number of options with intricate details.
Effectiveness of Presentation Formats
The effectiveness of a presentation format depends on several factors, including the complexity of the options, the number of options, and the user’s prior knowledge and experience. For instance, a grid format can effectively display multiple attributes of each option side-by-side, facilitating comparisons. A summary format can condense key information, allowing users to quickly grasp the essential characteristics of each option.
The clarity and conciseness of the presentation directly influence user comprehension and decision-making.
Table Illustrating Pros and Cons of Presentation Methods
| Presentation Method | Pros | Cons |
|---|---|---|
| Lists | Simple, easy to understand, quick overview. | Can become overwhelming for many options, lacks visual comparison. |
| Grids | Excellent for comparing multiple attributes, visual clarity. | Can be complex for users unfamiliar with grids, requires careful design. |
| Summaries | Concise, highlights key information, suitable for many options. | May lose some detail, requires careful selection of key information. |
| Interactive Comparisons | Users can directly compare options, more engaging. | Can be complex to develop, requires more technical skills. |
Identifying User Needs and Preferences
Understanding user needs and preferences is crucial for an agent to effectively tailor the presentation of diverse options. A good agent doesn’t just offer a list; it actively seeks to understand the user’s context, goals, and constraints. This understanding allows the agent to prioritize and present options that are most relevant and desirable to the user.Identifying user needs goes beyond simply gathering information.
It requires an agent to interpret the information, recognizing underlying motivations and implicit desires. This deeper understanding is essential for delivering a truly personalized experience, ensuring the options presented align with the user’s unique circumstances.
Real estate agents are amazing at showcasing a variety of options, and that includes different architectural styles. If you’re looking for something truly unique, exploring the offerings from the largest architectural firms, like those featured on largest architectural firms 2 , can be a great starting point. Ultimately, a good agent will help you navigate these options, highlighting the specific designs that best suit your needs and preferences.
Methods for Identifying User Needs
Agents can employ various methods to ascertain user needs and preferences. This involves gathering information from various sources and combining it to create a comprehensive profile of the user. These methods include, but are not limited to, explicit statements, inferred needs, and context-aware analysis.
- Explicit Statements: Users often articulate their needs directly. This could be through explicit requests, preferences, or feedback provided during the interaction. For example, a user might explicitly state a need for a fast delivery option or a specific price range. This direct input is invaluable in shaping the presentation.
- Inferred Needs: Sometimes, user needs are not explicitly stated. Agents can infer them based on past behavior, patterns, and contextual information. For instance, if a user consistently selects options within a particular price range, the agent can infer a preference for budget-friendly choices.
- Context-Aware Analysis: Agents should consider the context of the interaction to infer user needs. This includes factors like the time of day, location, or the user’s previous interactions with the system. For example, an agent might infer a preference for a local delivery option if the user is located in a specific city.
Learning and Adapting to User Preferences
Agents should not only identify initial preferences but also continuously learn and adapt to evolving preferences during the interaction. This dynamic learning process allows the agent to provide increasingly relevant and personalized options.
- Iterative Feedback: Agents can gather feedback throughout the interaction. This feedback, whether explicit or implicit, helps agents refine their understanding of the user’s needs and preferences. For example, if a user repeatedly selects options with a specific feature, the agent can infer a preference for that feature and subsequently highlight similar options in future presentations.
- Dynamic Adjustment: Agents should adjust their presentation dynamically based on user interactions. If a user expresses dissatisfaction with a presented option, the agent can adjust the presentation to offer alternatives. This continuous feedback loop ensures the agent’s presentation aligns with the user’s evolving needs.
Role of Data Analysis in Understanding User Preferences
Data analysis plays a pivotal role in understanding user preferences for diverse options. By analyzing vast amounts of user data, agents can identify patterns and trends that reveal valuable insights into user behavior.
- Pattern Recognition: Data analysis helps identify patterns in user choices. For example, if users consistently choose options within a specific price range, it indicates a preference for budget-friendly options.
- Trend Identification: Data analysis can reveal trends in user preferences over time. This helps agents understand how user preferences might be changing and adapt their presentation accordingly. For instance, if a particular option becomes more popular over a period, the agent can prioritize its presentation.
Examples of Dynamic Adjustment, Agents can help show diversity of options
Agents can dynamically adjust their presentation based on user interactions in real-time.
- Filtering Options: If a user expresses a preference for a specific feature, the agent can filter the presented options to show only those with that feature.
- Prioritizing Options: If a user repeatedly selects a specific option type, the agent can prioritize its presentation in subsequent interactions.
- Recommending Alternatives: If a user expresses dissatisfaction with an option, the agent can offer alternative options tailored to the user’s preferences.
Agent Capabilities for Handling Diverse Options
Agent capabilities are crucial for a smooth user experience when presented with numerous choices. Effective agents must not only understand the variety of options but also present them in a clear, concise, and user-friendly manner. This requires a robust system that can handle diverse data types and adapt to changing user needs. The ability to scale with increasing option availability is also essential for maintaining performance and user satisfaction.Agents must possess sophisticated knowledge representation and reasoning capabilities to process and present diverse information effectively.
This includes understanding user preferences, identifying relevant options, and filtering out irrelevant choices. Further, agents must be able to present these options in a manner that is easily digestible and actionable for the user.
Travel agents are amazing at showcasing a wide range of options, from budget-friendly getaways to luxurious escapes like the recent $40 million rebirth of the Ritz-Carlton St. Thomas. This impressive investment highlights the diversity of experiences available, and a good agent can help you find the perfect fit for your needs and desires. They can navigate the details and ensure you get the best deal, whether it’s a splurge or a more modest trip.
Technical Requirements for Managing Diverse Data
Agents need to handle diverse data types, including structured data (databases), unstructured data (text, images, audio), and semi-structured data (XML, JSON). This requires robust data processing pipelines that can transform different formats into a unified representation. The agents should also be able to handle various data sizes and formats to support diverse options. For instance, an agent recommending movies should be able to manage data from different sources, such as user ratings, critical reviews, and plot summaries.
These data sources could use various formats and structures, requiring the agent to perform data transformations and mappings to a common internal representation.
Scalability for Handling Increasing Options
Scalability is critical for agents to handle a growing number of options. This means the agent’s ability to process and present options must increase proportionally with the number of options. An agent recommending products from an online store should be able to handle millions of products and their attributes. This involves utilizing distributed computing systems, efficient algorithms, and robust data structures to ensure the agent can quickly and accurately deliver relevant options to users.
Travel agents aren’t just for booking flights anymore; they can open up a world of possibilities, showcasing a diverse range of options for your trip. For example, if you’re planning a trip to Saudi Arabia, understanding the 6 key planning tips found on 6 key planning tips for travel to Saudi Arabia is crucial. From visa requirements to cultural sensitivities, they can guide you through the nuances, ensuring a smoother and more enriching experience.
Ultimately, agents can provide insights into a multitude of experiences, not just for Saudi Arabia, but many other destinations, helping you find the perfect fit for your travel style.
For example, a recommendation system for an e-commerce site needs to maintain performance as the product catalog expands, ensuring the system doesn’t slow down or fail under pressure.
Organizing and Presenting Diverse Information
Agents must organize and present diverse information in a user-friendly manner. This includes filtering, sorting, and grouping options based on user preferences and needs. Presentation should include clear visual cues and intuitive navigation to allow users to easily explore and understand the available options. For example, an agent providing travel recommendations should group flights, hotels, and activities based on price, location, and user preferences.
This organization needs to be dynamic and adapt to changing user preferences in real-time. Visual elements like charts, graphs, and interactive maps can help users quickly grasp complex information and make informed decisions.
Illustrative Examples of Agents and Diverse Options
Agents are increasingly capable of presenting users with a wide array of options, tailoring recommendations to individual preferences and needs. This empowers users to make informed decisions and explore diverse possibilities. A well-designed agent goes beyond simply listing options; it actively guides users through the decision-making process, highlighting potential trade-offs and benefits of each choice.This exploration dives deeper into practical examples of how agents can showcase diverse options, demonstrating their effectiveness in different contexts.
We’ll analyze scenarios where agents present varied options and discuss the considerations for successful implementation.
Travel Planning Agents and Diverse Options
Travel planning agents can leverage diverse options to cater to different user preferences. Consider a user seeking a beach vacation in the Caribbean. A good agent would present various options beyond simply listing resorts. For instance, it could offer eco-friendly accommodations, boutique hotels, all-inclusive resorts, or options with varying activity levels. Furthermore, the agent might highlight the potential for cultural experiences, local cuisine, and unique excursions.
Product Recommendation Agents and Diverse Options
Product recommendation agents can personalize recommendations to user needs and preferences. For example, a user interested in a new laptop might receive options ranging from budget-friendly models to high-end gaming laptops, as well as options for different operating systems. An effective agent would also present different levels of technical specifications, such as battery life, processing power, and storage capacity.
Moreover, the agent can present reviews, ratings, and user feedback on each option to aid the user’s decision-making.
Scenarios for Agent Presentation of Diverse Options
| Scenario | Diverse Options Presented | User Needs Addressed |
|---|---|---|
| Booking a flight | Different airlines, flight times, baggage allowances, and seat types | Cost-conscious travelers, those prioritizing comfort or speed, or those with specific baggage needs |
| Finding a restaurant | Various cuisines, price ranges, dietary restrictions, and reviews | People seeking a specific cuisine, budget-conscious diners, or those with allergies or dietary preferences |
| Purchasing a new phone | Different models, operating systems, storage capacities, and camera quality | Users with diverse budgets, those prioritizing camera quality, or those who want specific operating systems |
Challenges and Considerations
Presenting diverse options effectively involves careful consideration of several factors. One challenge is ensuring that the options presented are truly diverse and not simply variations on a theme. Another consideration is presenting options in a clear and concise manner, avoiding overwhelming the user with too much information. Furthermore, the agent must consider the user’s context and preferences, ensuring that the presented options align with their specific needs and desires.
Effective Agents Presenting Diverse Options
Several agents excel at presenting diverse options. For example, Amazon’s product recommendations consistently offer a broad range of products tailored to user preferences. Netflix’s movie and show suggestions also demonstrate diverse options catering to various genres and tastes. These agents demonstrate the potential for effective presentation of diverse options in different contexts.
The Impact of Agent-Presented Diversity
Agent-powered systems are increasingly capable of presenting users with a wide array of options, tailored to individual needs and preferences. This ability to showcase diverse choices significantly impacts the user experience, leading to greater satisfaction and engagement. Understanding this impact is crucial for designing effective and user-friendly agents.Presenting diverse options is more than just a feature; it’s a fundamental shift in how agents interact with users.
It empowers users by giving them a wider range of choices, moving beyond simple, pre-defined solutions. This fosters a more collaborative and dynamic interaction, where the user feels actively involved in shaping the outcome.
Enhanced User Experience
Presenting diverse options leads to a richer and more personalized user experience. Users appreciate the agency they feel when presented with options tailored to their specific needs and preferences. This active participation contributes to a more engaging and satisfying interaction.
Improved User Satisfaction and Engagement
Diverse options empower users to feel more in control and satisfied with the outcome. The sense of choice and agency boosts engagement, leading to increased user satisfaction. By tailoring options to individual needs, agents can foster a deeper connection with users, leading to higher satisfaction rates and increased use of the system. This is especially true in complex tasks where users might have difficulty choosing the best course of action on their own.
Benefits of Using Agents for Broader Options
Agents can access and process a vast amount of information, enabling them to present a much broader range of options than humans could manage alone. This wider range of choices allows users to consider solutions they might have otherwise overlooked. This is particularly valuable in complex decision-making processes, where multiple factors and potential outcomes need to be considered. An agent can analyze user history, preferences, and contextual information to recommend options that are highly relevant and beneficial.
Potential Pitfalls and Mitigation Strategies
Presenting a multitude of options can sometimes overwhelm users, leading to indecision and dissatisfaction. This is a common problem in complex systems with many variables. Strategies to mitigate this include:
- Filtering and Prioritization: Agents should prioritize and filter options based on user needs and preferences, presenting only the most relevant choices. This ensures users are not overwhelmed by irrelevant or less suitable options.
- Clear and Concise Explanations: Providing clear explanations for each option helps users understand the implications and trade-offs involved. This reduces ambiguity and allows for informed decision-making.
- Progressive Disclosure: Presenting options in stages, starting with a smaller set and progressively expanding based on user interaction, can help manage the cognitive load. This method prevents initial overload and allows for a more focused approach.
- Feedback Mechanisms: Including feedback mechanisms that allow users to refine their preferences or request clarification on options can improve the overall experience. This constant interaction ensures the agent is providing valuable and relevant options.
Presenting diverse options can lead to a more satisfying and engaging user experience. By carefully considering potential pitfalls and implementing effective mitigation strategies, agents can provide a powerful and beneficial tool for users in a wide variety of applications.
Evaluating the Effectiveness of Diverse Option Presentation
Assessing the effectiveness of agents presenting diverse options goes beyond simply offering choices. It requires a structured methodology to measure user satisfaction, agent performance, and the overall impact of the presented options on user outcomes. This evaluation process provides crucial insights for refining agent design and improving user experience.Understanding user needs and preferences is paramount to judging the efficacy of the agent’s presentation.
A well-designed evaluation process can pinpoint areas where the agent excels and where improvements are necessary.
Methodology for Evaluating Agent Effectiveness
A robust methodology for evaluating diverse option presentation involves a multi-faceted approach. It must consider user feedback, objective metrics, and the agent’s ability to adapt to varying user needs. This approach ensures a comprehensive understanding of the agent’s performance.
Measuring User Satisfaction
User satisfaction with diverse option presentation is a key component of the evaluation. Collecting user feedback is critical. Methods include surveys, interviews, and feedback forms that explicitly ask users about their experience with the presented options. The surveys should be structured to allow for nuanced responses and identify specific aspects of the presentation that users found helpful or unhelpful.
Agents are amazing for showing you all the different options available, especially when it comes to finding the best deals on office supplies. Knowing how to stay on top of your office packaging shipping supplies costs is key, and having an agent who can compare quotes for you can save a lot of time and headaches. They’re truly invaluable in helping you navigate the vast array of choices out there!
Qualitative data collected through interviews can provide deeper insights into user experiences and motivations.
Metrics for Evaluating Agent Performance
Various metrics can gauge the performance of agents in presenting diverse options. These metrics should encompass aspects of the agent’s presentation style, its ability to adapt to user needs, and the quality of the options presented. Key performance indicators (KPIs) include the time taken to present options, the accuracy of the options presented in relation to user needs, and the diversity of options provided.
Agent Performance Evaluation Criteria
| Criteria | Description | Measurement Method |
|---|---|---|
| Option Relevance | How well do the presented options align with the user’s stated or inferred needs? | Percentage of options chosen by users that match their expressed needs. |
| Option Diversity | How varied and comprehensive are the presented options? | Qualitative analysis of option breadth and depth, comparing the presented options to a pre-defined set of possible options. |
| Presentation Clarity | How easy is it for the user to understand and interpret the presented options? | User feedback surveys measuring clarity and comprehension of options. |
| Presentation Time | How quickly does the agent present the options? | Average time taken to present options, including response times to user queries. |
| User Engagement | How actively does the user interact with the presented options? | Number of options explored, time spent on each option, and user feedback on the presentation’s engagement level. |
Final Review
In conclusion, agents play a crucial role in showcasing the diversity of options available to users. By understanding user needs, employing effective presentation strategies, and leveraging the right technologies, agents can enhance user satisfaction and engagement. This comprehensive approach ensures users are not only presented with a multitude of choices but also have their unique preferences considered, leading to more meaningful and personalized experiences.
Essential Questionnaire
What are some common pitfalls in presenting diverse options?
Overwhelming users with too many choices, failing to consider individual preferences, and presenting options in a disorganized or confusing manner are common pitfalls. Effective agents address these by filtering choices, personalizing presentations, and organizing options in a user-friendly way.
How can agents dynamically adjust their presentation based on user interactions?
Agents can track user preferences and behaviors to dynamically adjust their presentation. For example, if a user frequently selects certain types of options, the agent can prioritize those options in future presentations. This personalization improves user satisfaction by showing relevant items.
What role does data analysis play in understanding user preferences for diverse options?
Data analysis helps agents understand user preferences by identifying patterns and trends in user behavior. This data allows agents to learn from past interactions and tailor future presentations to better meet user needs and desires.






